Study identifies chlorcyclizine as a potential treatment to reduce protoporphyrin-IX accumulation and liver damage in experimental models of EPP.
 Study: The histamine pathway is a target to treat hepatic experimental erythropoietic protoporphyria. Image Credit: luchschenF/Shutterstock.com
Study: The histamine pathway is a target to treat hepatic experimental erythropoietic protoporphyria. Image Credit: luchschenF/Shutterstock.com
In a recent study published in the Cellular and Molecular Gastroenterology and Hepatology, a group of researchers evaluated the role of the histamine pathway in protoporphyrin-IX (PP-IX) accumulation and assessed the therapeutic potential of chlorcyclizine and antihistamines for treating liver disease in erythropoietic protoporphyria (EPP) (a genetic disorder causing PP-IX buildup, leading to photosensitivity).
Background
EPP results from reduced ferrochelatase activity, causing PP-IX accumulation in the liver and erythroid precursors. While skin photosensitivity is the primary symptom, 10-25% of patients develop liver dysfunction, with 1-4% progressing to end-stage liver failure requiring transplantation.
Current treatments alleviate skin symptoms but fail to address liver disease, leaving a critical therapeutic gap. Histamine and mast cells have been implicated in liver pathology, suggesting novel intervention targets.
Further research is essential to explore the mechanistic role of the histamine pathway and its potential for developing targeted therapies for EPP-associated liver disease.
About the study
In the present study, the methods involved high-throughput drug screening using a zebrafish model to identify compounds that reduce PP-IX accumulation. Transgenic zebrafish larvae were injected with δ-aminolevulinic acid (ALA) and deferoxamine (DFO), inducing PP-IX overproduction.
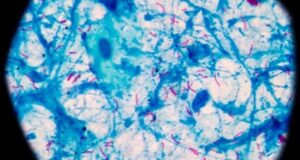
Fluorescence imaging was used to assess liver PP-IX levels, leading to the identification of chlorcyclizine (CCZ) as a promising compound.
Validation studies were conducted in primary mouse hepatocytes treated with ALA and DFO and in two mouse models of EPP- the Ferrochelatase mutant 1 with a pedigree from Pas (Fechm1Pas) mice and mice fed with a porphyrinogenic diet containing 3,5-diethoxycarbonyl-1,4-dihydrocollidine (DDC).
Plasma, liver, and stool PP-IX levels were measured using fluorescence, and histological analysis assessed liver morphology. Nuclear translocation of key bile acid receptors, including constitutive androstane receptor and farnesoid-X receptor, was analyzed, along with the expression of PP-IX clearance transporters.
Knockdown experiments targeting bile salt export pump (BSEP) and multidrug resistance-associated protein-4 (MRP4) explored transporter roles in PP-IX handling.
The study further investigated histamine receptor (H) activity using antihistamines, assessing their effect on PP-IX levels and protein aggregation.
Data were statistically analyzed to confirm the efficacy of CCZ in lowering PP-IX and alleviating EPP-related liver damage, highlighting the potential therapeutic value of antihistamines.
Study results
The results revealed that CCZ effectively reduces PP-IX accumulation in multiple experimental models of EPP. In zebrafish, CCZ significantly decreased hepatic PP-IX fluorescence and increased its excretion into the surrounding medium. Similarly, CCZ treatment in primary mouse hepatocytes led to a dose-dependent reduction in intracellular PP-IX levels, confirming its efficacy in vitro.
In Fechm1Pas mice, CCZ administration resulted in a notable reduction of hepatic PP-IX deposits, particularly medium-sized deposits, in female mice. The compound also decreased PP-IX levels in the liver, erythrocytes, and bone marrow of female mice while promoting stool excretion of PP-IX.
Plasma biomarkers of liver injury, such as alanine aminotransferase (ALT) and alkaline phosphatase (ALP), were also reduced following CCZ treatment in female mice. However, male mice did not exhibit similar reductions, indicating a sex-specific response.
CCZ was further tested in DDC-fed mice, a pharmacological model of EPP. Female mice exhibited higher PP-IX accumulation than males, which is consistent with previous findings. CCZ effectively reduced hepatic PP-IX levels and mitigated liver injury in females but not males.
These effects correlated with a decrease in protein oxidation and aggregation, suggesting improved cellular stress responses.
Histamine was identified as a pro-porphyrinogenic factor in hepatocytes. Both H1- and H2-receptor blockade were shown to decrease PP-IX levels. CCZ treatment reduced hepatic mast cell infiltration and histamine levels, with more pronounced effects observed in female mice.
The findings suggest that histamine and its signaling pathways play a critical role in PP-IX accumulation and EPP-related liver pathology.
Further mechanistic studies revealed that CCZ induced nuclear translocation of constitutive androstane receptor (CAR) and farnesoid X receptor (FXR), enhancing bile acid transporter expression, including MRP4 and BSEP.
This pathway likely facilitates PP-IX clearance through bile excretion. Knockdown experiments of MRP4 and BSEP confirmed their role in reducing PP-IX-associated protein aggregation.
Conclusion
To summarize, only afamelanotide (SCENESSE®), an α-melanocyte-stimulating hormone analog, has been Food and Drug Administration (FDA)-approved to address skin symptoms in EPP, leaving liver complications untreated. CCZ, an H1-antihistamine, was identified through drug screening as a potent PP-IX reducer.
CCZ decreased PP-IX levels and alleviated liver injury in female experimental models by inducing bile excretion through activation of CAR/MRP4 and FXR/BSEP pathways. It also inhibited histamine-mediated PP-IX accumulation, reduced protein aggregation, and oxidative stress.
These findings suggest CCZ and other antihistamines hold promise as safe and effective treatments for EPP-related liver disease.
Journal reference:
-
Kuo N, Li P, Cunha JB, Chen L, et al. (2025) The histamine pathway is a target to treat hepatic experimental erythropoietic protoporphyria. Cellular and Molecular Gastroenterology and Hepatology. doi: https://doi.org/10.1016/j.jcmgh.2025.101463.