Lissencephaly is a spectrum of rare, genetic disorders in which the brain fails to develop its hallmark folds. The disorders are often associated with seizures and intellectual disability and currently there are no available treatments.
A new Yale study, however, has identified a molecular mechanism that underlies some lissencephaly disorders — and a drug that prevents and reverses lissencephaly malformations in organoids (small, three-dimensional replicas of developing brains that allow scientists to study early brain development).
The findings, reported Jan. 1 in Nature, may point to a target for treatment, researchers say.
Lissencephaly belongs to a group of disorders we call malformations of cortical development, meaning the normal development and structure of the brain is disrupted. They come about because certain genes that are very important for brain development are affected by rare mutations.”
Angeliki Louvi, professor of neurosurgery and of neuroscience, Yale School of Medicine (YSM) and co-senior author of the study
The new study builds on gene discovery research conducted by the Yale Program in Neurogenetics and pioneered by co-senior author Murat Gunel, Sterling Professor of Neurosurgery and professor of genetics and of neuroscience at YSM. For years, the program has collected blood samples from patients affected by brain malformations in order to identify genetic mutations associated with their disorders.
“It has been 17 years since the first family enrolled in our research, and they happen to be one of the families in the study,” said Kaya Bilguvar, associate professor adjunct of neurosurgery and genetics at YSM, and co-senior author of the study. “This level of collective commitment, including by patients and families, is inspiring.”
Past research has connected a number of genes to lissencephaly, but there are some patient cases where the genetic causes remain unknown. Further, how these genetic mutations actually lead to lissencephaly at the molecular level has not been well understood.
For the new study, researchers found a new gene associated with lissencephaly and then developed brain organoids from the cells of patients with two different types of lissencephaly. Specifically, they took cells from strands of the patients’ hair and, through a chemical method, reversed the cells’ development, pushing them into an earlier, unspecialized cell stage. The researchers then reprogrammed the cells to become neurons, which grew together to form three-dimensional organoids.
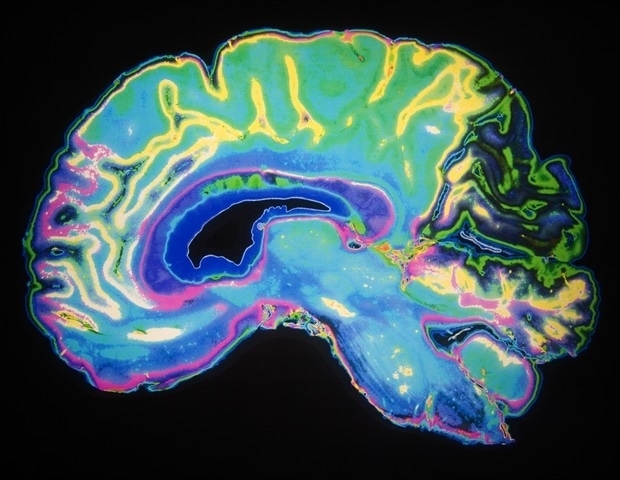
Along with having little to no folding in their brains, individuals with lissencephaly also have a thicker than usual cerebral cortex. The organoids grown from the patients’ cells for the new study also developed thicker cortex-like structures than healthy organoids, much like what’s observed in lissencephaly, researchers found.
The research team also performed several analyses to evaluate the gene and protein expression levels in the organoids. Their findings pointed to dysregulation in the mTOR (mammalian target of rapamycin) pathway in both types of lissencephaly organoids they were studying.
“This is a fundamental pathway that governs many different aspects of cellular metabolism to maintain cellular homeostasis,” said Louvi. “And we know of many disorders in which the mTOR pathway is overactive, but here we found that in lissencephaly it’s actually underperforming.”
Ultimately, the researchers exposed the organoids to a drug that boosts mTOR pathway activity and found that it could prevent and reverse thickening of the organoid cortical plate-like area depending on when it was introduced.
“Right now, in medicine we have no way to slow or reverse these structural brain malformations in lissencephaly either during pregnancy or after,” said lead author Ce Zhang, who was an M.D.-Ph.D. student in the Bilguvar and Louvi labs and will soon begin neurology residency at Ceders-Sinai in Los Angeles. “That limits us to treating the symptoms, but even that can be difficult, as lissencephaly seizures may not be well-controlled using typical anti-epileptic drugs.”
But since the study showed that the mTOR pathway is implicated in two different types of lissencephaly, it suggests this might be the case for additional types of lissencephaly — or maybe even the entire spectrum of lissencephaly disorders.
“If there’s a converging pathway shared between these disorders, regardless of the genetic cause, it could mean one treatment, such as a mTOR activator like the one we tested in the study, might be beneficial to patients across the lissencephaly spectrum,” said Zhang.
Going forward, the researchers aim to determine whether the mTOR pathway is implicated in other genetic types of lissencephaly and dig deeper into how an underactive mTOR pathway leads to lissencephaly.
“These findings extend our knowledge of this pathway, highlighting the fine balance that has to be met for healthy brain development,” said Louvi. “Now we want to understand what exactly happens molecularly when mTOR is underactivated.”
It will be important to explore potential clinical applications of mTOR activators in this spectrum of disorders as well, Bilguvar added, as benefiting patients though basic discoveries is the program’s ongoing motivation.
Source:
Journal reference:
Zhang, C., et al. (2025) Dysregulation of mTOR signalling is a converging mechanism in lissencephaly. Nature. doi.org/10.1038/s41586-024-08341-9.