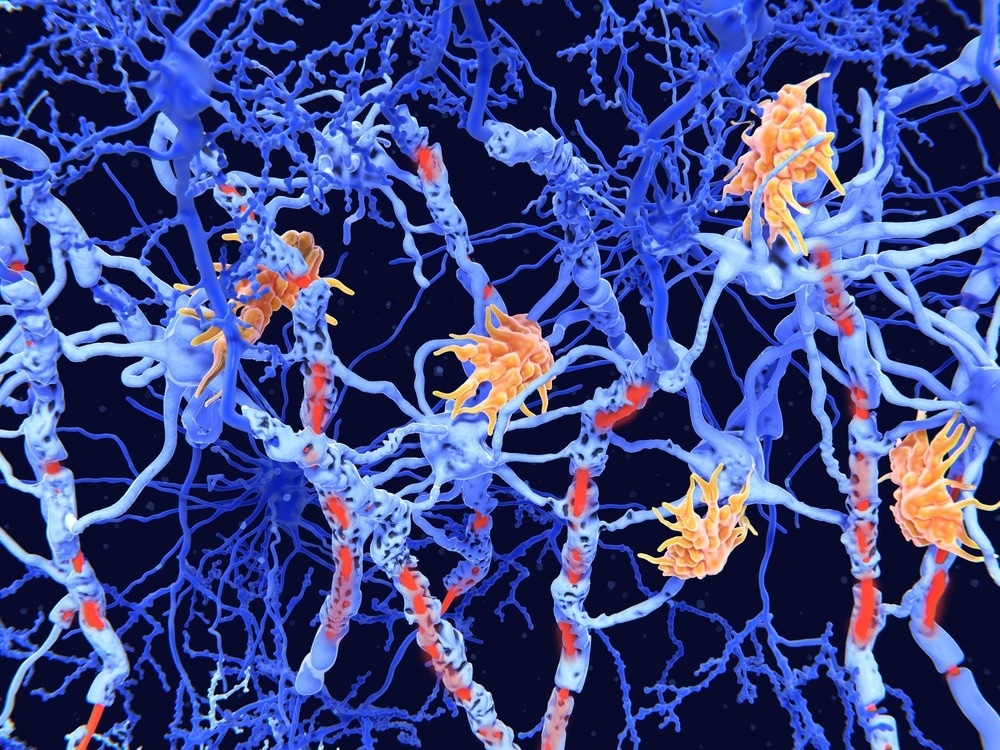
Breakthrough research details how distinct tissue niches and cell communication contribute to chronic active lesions in MS.
In a recent study published in Nature Neuroscience, researchers used single-nucleus ribonucleic acid (RNA) sequencing (snRNAseq) and spatial transcriptomics (ST) on subcortical multiple sclerosis (MS) and control tissues to map cell types, interactions, and pathways in the lesion and non-lesion areas.
They identified specialized niches like inflamed lesion rims and the lesion core, revealing unique cell interactions, including cilia-forming astrocytes and cell communications that drive lesion progression in MS.
Background
MS is a leading inflammatory disease of the central nervous system, marked by demyelination, axonal damage, and chronic tissue changes, including neuronal loss and brain atrophy. Chronic MS is complicated by persistent, compartmentalized inflammation, especially at the rims of subcortical white matter lesions, which often exhibit iron accumulation and disease progression.
MS lesions progress in identifiable stages, beginning with active inflammation and myelin breakdown by immune cells; some lesions may undergo remyelination, while others advance to a chronic active phase with an inflammatory rim. In this stage, a dense glial scar forms, leading eventually to inactive lesions with minimal inflammation.
Although imaging and histopathology have provided insights into lesion progression, limitations in spatially precise molecular techniques have prevented detailed mapping of cell-type-specific pathology within distinct lesion and non-lesion areas.
In the present study, researchers used snRNAseq and ST to map cell types, molecular features, and cell interactions within subcortical MS lesions.
About the study
Researchers analyzed 12 MS lesion samples and seven control samples, focusing on chronic active (MS-CA) and chronic inactive (MS-CI) lesions based on markers like demyelination, inflammation, and iron uptake. The United Kingdom Multiple Sclerosis Tissue Bank at Imperial College London provided all the tissue samples. Both manual and computational annotations were used to identify distinct tissue niches, and pathway analysis was done to identify biological functions across regions.
Astrocytes (AS) were analyzed and validated through comparative datasets and marker analysis. Subtypes were mapped using ST and confirmed with single-molecule fluorescence in situ hybridization (smFISH) and immunofluorescence. The study also examined molecular differences in MS lesion types. Differential gene expression and relative abundances of cell types, particularly oligodendrocytes (OL), AS, and myeloid cells (MC), were analyzed. Cell-cell communication (CCC) events were inferred by pairing snRNA-seq and ST data, revealing lesion-specific ligand-receptor interactions. These interactions were further validated with smFISH, revealing cell type- and lesion type-specific signaling pathways.
Results and discussion
Nine main cell types and 79 subtypes were identified, with AS being a key focus. Notably, a unique “ciliated” AS subtype was discovered, overrepresented in lesion cores, associated with the glial scar, and validated by cilia-related markers and gene expression analysis. This subtype expressed FOXJ1 (forkhead box J1), a key gene in cilia biogenesis, and displayed large cilia structures, suggesting its role in lesion remodeling.
Spatial analysis revealed distinct tissue niches, including the lesion core, rim, and perivascular regions. A high abundance of AS was found in the lesion core, while OL was more prevalent in control regions.
Pathway analysis indicated active tissue remodeling and immune signaling in MS lesions, particularly at lesion rims, with inflammation-related pathways such as JAK-STAT (Janus kinase/signal transducers and activators of transcription) and TNF (tumor necrosis factor) signaling enriched. A vascular-infiltrating niche, characterized by immune and endothelial cells, was identified, highlighting ongoing inflammation in MS-affected tissue.
The study also examined differences between MS-CA and MS-CI lesions at the molecular and cellular levels. MS-CA lesions showed greater gene dysregulation in OL, AS, and MC, with pathways related to inflammation, tissue remodeling, and stress. In contrast, MS-CI lesions had OLs expressing genes related to lipid regulation and tissue remodeling, while AS in MS-CI lesions showed scar-forming activity.
MCs in MS-CA lesions were found to be linked to inflammation, while those in MS-CI lesions were involved in tissue maintenance. Lesion areas like the lesion rim and lesion core had distinct expression profiles, with inflammation in MS-CA and cell integrity pathways in MS-CI.
Additionally, the researchers identified 190 significant differential CCC events, primarily involving AS, MC, and OL. MS lesions, especially MS-CA, showed immune-driven CCC networks and interactions such as HMGB1-CD163/TLR2 and CD14-ITGB1 were validated in the lesion rim.
These interactions were absent in control and indicated key roles for MC in MS pathology, particularly in inflammation and tissue remodeling. Overall, this comprehensive analysis provides insights into the cellular and molecular differences between MS lesion types, revealing potential signaling pathways critical to MS progression.
Conclusion
In conclusion, the study provides valuable insights into the complex microenvironment driving MS lesion progression, particularly at lesion rims, identifying cell-type-specific and spatially restricted drivers of pathology. While further research on various lesion types and patient-specific factors is needed, these findings advance understanding of the molecular structure in MS lesions. Functional validation of these findings is warranted in future studies.




