New study reveals how lingering spike protein in the brain’s borders could explain long-term COVID-19 neurological symptoms and highlight vaccines’ protective role.
 Study: Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19. Image Credit: sciencepics / Shutterstock
Study: Persistence of spike protein at the skull-meninges-brain axis may contribute to the neurological sequelae of COVID-19. Image Credit: sciencepics / Shutterstock
In a recent study published in the journal Cell Host & Microbe, researchers investigated the persistence of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) spike protein at the skull-meninges-brain axis and its role in neurological sequelae associated with coronavirus disease 2019 (COVID-19).
Background
SARS-CoV-2 infection is linked to various neurological complications, including brain fog, reduced gray matter thickness, and heightened stroke risk, even in mild cases. While virus Ribonucleic Acid (RNA) is inconsistently detected in brain tissues, widespread immune activation is observed, suggesting indirect mechanisms.
The SARS-CoV-2 spike protein, one of the virus’s key structural components, triggers inflammatory responses via Toll-like receptors, affects endothelial function, and forms proinflammatory clots.
Recent evidence suggests that it persists in immune cells and plasma for extended periods, which has prompted further research. Understanding its distribution and functional impact on the brain and other organs could shed light on both acute and chronic neurological sequelae of COVID-19.
About the Study
SARS-CoV-2 Omicron and SARS-CoV-2 green fluorescent protein (GFP)-tagged virus strains were prepared and utilized for infection studies in mice. Transgenic K18-human angiotensin-converting enzyme 2 (K18-hACE2) mice and wild-type C57BL/6J mice were aerosol-inoculated with specific viral titers to assess the virus’s impact. Immunization protocols involved the intramuscular administration of the BNT162b2 messenger RNA (mRNA) vaccine prior to viral exposure. Infected mice were observed for clinical symptoms, weighed daily, and euthanized at designated time points.
The study also included fluorescently labeled recombinant spike S1 protein injections to evaluate its systemic and localized effects.
During intravenous and skull marrow microinjection procedures, anesthesia was induced, and injections were targeted to both peripheral tissues and the spongy bone marrow of the skull. Following injections, tissue perfusion was conducted using phosphate-buffered saline (PBS) and paraformaldehyde (PFA) to achieve fixation for subsequent analyses. Tissue clearing via the three-dimensional imaging of solvent-cleared organs (3DISCO) protocol rendered mouse tissues optically transparent, facilitating detailed imaging of viral protein distribution with advanced microscopy.
High-resolution imaging methods, including confocal microscopy, allowed precise visualization of human brain and skull tissues. Immunofluorescence, laser capture microdissection, and mass spectrometry provided insights into proteomic changes and inflammatory pathways associated with spike protein persistence.
Behavioral assessments, ischemia models, and traumatic brain injury (TBI) experiments evaluated the functional consequences of spike protein persistence in the brain and peripheral tissues. Comprehensive statistical analyses validated the findings, ensuring accurate interpretations of the data.
Study Results
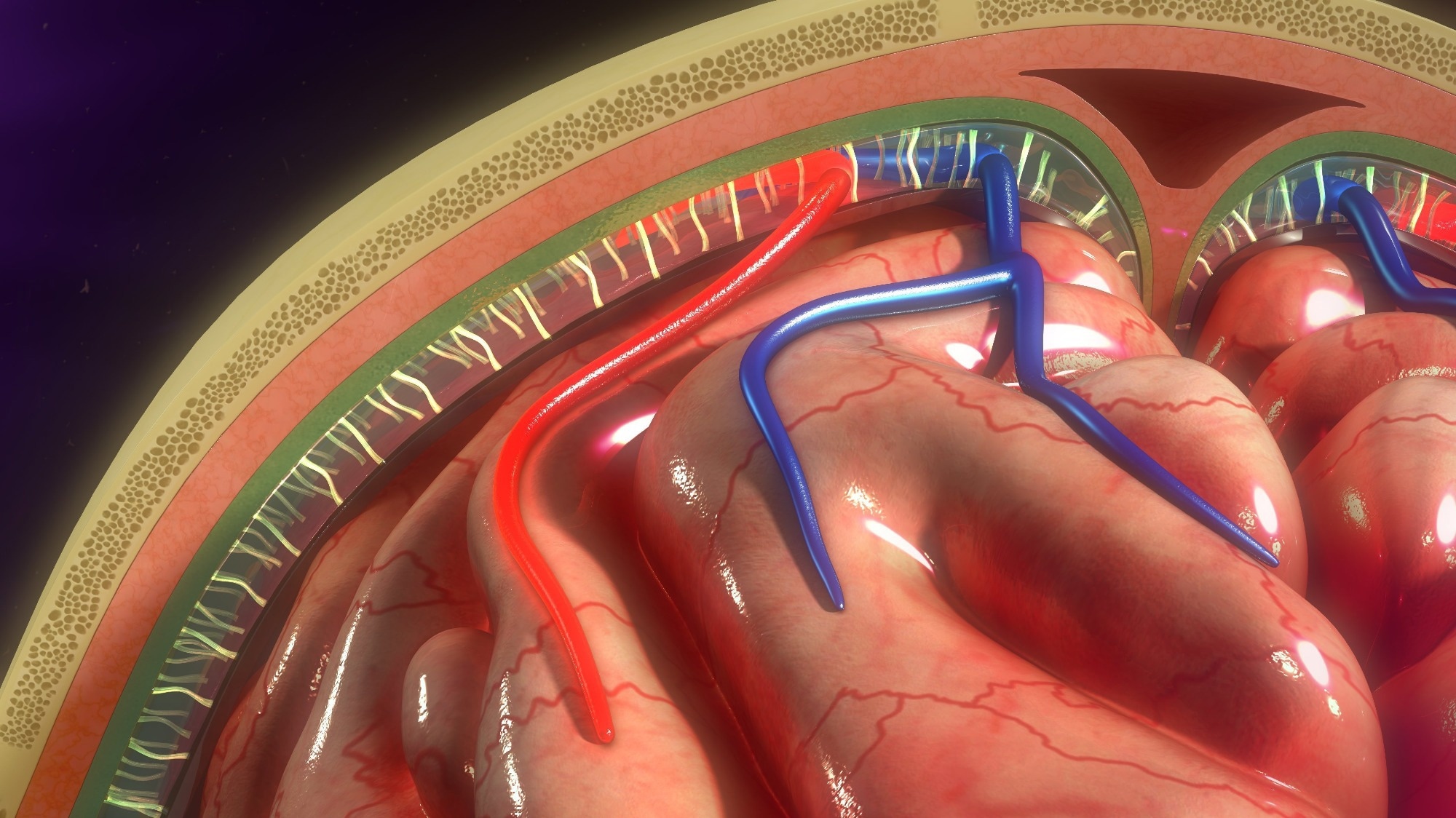
The study revealed a persistent presence of the SARS-CoV-2 spike protein in the skull, meninges, and brain of COVID-19 patients, shedding light on the virus’s potential neurological impacts.
Using advanced tissue clearing and imaging techniques, researchers detected the spike protein in the skull marrow, recently discovered skull-meninges connections (SMCs), and meninges of patients who died from acute COVID-19. In the skull marrow, 45% of the spike protein was found outside blood vessels, suggesting extravasation into the tissue.
Additionally, 27% of the spike protein colocalized with ionized calcium-binding adaptor molecule 1 (Iba1)-positive myeloid cells. Spike protein was also detected in the perinuclear space of meningeal cells and near NeuN-positive neurons in the brain’s frontal cortex, indicating its interaction with neuronal regions.
Interestingly, while SARS-CoV-2 RNA was often undetectable in brain samples, spike protein persisted, suggesting a longer half-life or a unique uptake mechanism distinct from active viral replication. In non-COVID-19 deaths, spike protein persisted in skull marrow samples long after infection, correlating with elevated levels of tau protein, neurofilament light chain (NfL), and glial fibrillary acidic protein (GFAP) in cerebrospinal fluid (CSF) of long COVID patients. These markers indicate ongoing neurodegeneration, supporting the hypothesis that spike protein contributes to chronic neurological symptoms.
Mouse models confirmed these findings, with SARS-CoV-2 infection resulting in spike protein distribution across various organs, including the skull marrow and brain cortex, even after viral RNA diminished. The spike protein was also shown to cross the blood-brain barrier (BBB) and localize in ACE2-expressing tissues.
Proteomic analysis revealed significant changes in skull marrow, meninges, and brain cortex tissues, implicating pathways like neutrophil extracellular traps (NETs), mitogen-activated protein kinase (MAPK), and phosphoinositide 3-kinase (PI3K)-protein kinase B (AKT) signaling. These changes were particularly prominent in areas with spike protein, contributing to lysosomal activation, axonal damage, and neurodegeneration-related markers.
Functional studies confirmed the pathological effects of the spike protein. Microinjection into the skull marrow triggered neuroinflammation, neuronal damage, and lysosomal activation. Behavioral experiments revealed spike protein-induced anxiety-like behavior in mice and exacerbation of TBI and stroke outcomes, leading to increased long-term brain damage.
Finally, mRNA vaccines reduced spike protein accumulation in mice, particularly in the brain and skull regions, though they did not eliminate it entirely.
Conclusions
To summarize, the long-term neurological effects of COVID-19, such as brain fog and tissue loss, are linked to persistent spike protein, systemic inflammation, and BBB disruption. Spike protein was detected in patients’ skulls, meninges, and brains, even in a polymerase chain reaction (PCR)-negative post-mortem samples, suggesting prolonged protein presence. Mouse studies revealed spike protein accumulation in skull marrow and SMCs, inducing inflammation, anxiety-like behavior, and worsened outcomes in brain injury models.
Advanced proteomic analyses highlighted shared markers with neurodegenerative diseases like Alzheimer’s, underscoring the overlap with chronic neurological conditions. Vaccination reduced spike protein levels and associated inflammation, emphasizing its role in mitigating both acute and chronic effects.