If you were to tell me that at the beginning of the year, I would spend half of it going blind, having eye surgery and dealing with various post-op complications, I would have laughed. No, seriously, I would not have believed you. But somehow, that is exactly what happened. At 24 years old, I went blind, had eye surgery and spent more time at my doctor’s office than at my neighborhood grocery store. My name is Carissa Mosness, I’m an assistant editor here at FIRST for Women and this is my very long experience with retinal detachment.
The beginning of my journey: recognizing retinal detachment symptoms
On July 28 this year, I noticed “floaters” in my right eye. Originally, I thought it was a dusty contact lens, so I replaced it and went about my day. It helped for a little bit, but then I noticed what appeared to be flashing lights in my eye—which was odd because I was sitting in bed reading. So, I did what any 24-year-old woman would do: I called my mother. She told me to give it a day or two, and then we could talk about possible options. Feeling better, I went to bed and thought nothing else of it.
The next day, the flashes and floaters were gone. But as I was getting ready, I realized that a lot of the room I was in had “disappeared”. Portions of my field of vision were just black. I didn’t have time to worry or think about it because I had to get to work. Besides, it was nothing like the flashers and floaters had been.
That night, though, after a long day of having no peripheral vision, the flashers came back. It was at that moment I recalled a warning an eye doctor had given me eight months prior at my annual check-up: If I experienced floaters and flashers, I should see a doctor right away to avoid losing my vision.
Getting diagnosed with retinal detachment
Four days after booking an appointment, I to realize that my right eye was basically nonfunctional. If something wasn’t directly in front of it, I couldn’t see it. And when I could see something, there was most likely a flasher or floater in front of it. I had essentially lost my vision that eye.
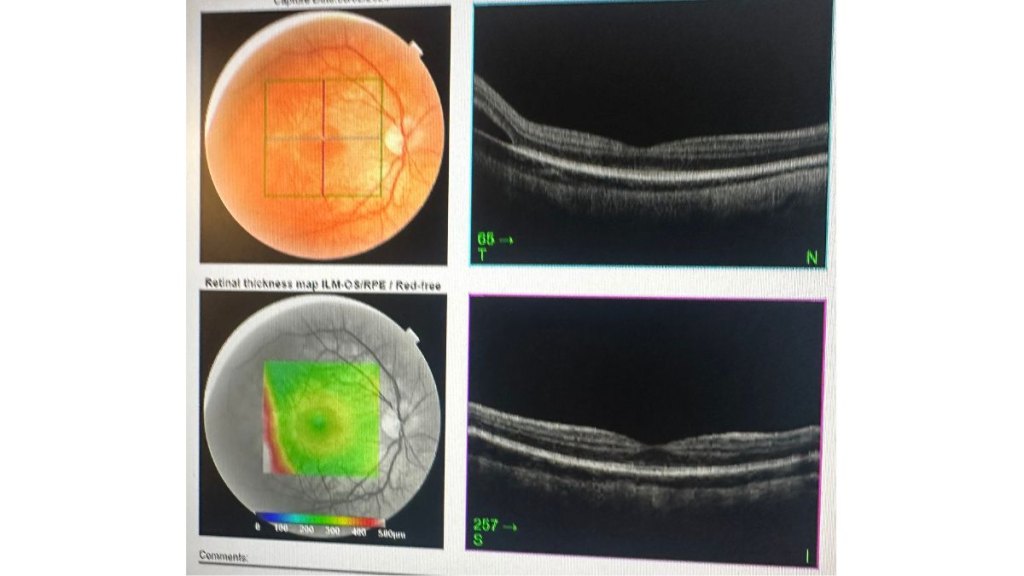
After a series of tests that involved me staring at various charts and pictures, having lights of all sizes flashed in my face and even an eye ultrasound, the doctor was able to tell me that I had a retinal tear in my right eye and needed to get it fixed right away. If I didn’t, I could lose my vision permanently.
A flurry of eye tests followed
Thankfully, my doctor had a connection at the best retina detachment center in the country, and it happened to be right down the street in New York City.
The next doctors thought they could fix the detachment quickly with a laser because of how soon after experiencing symptoms of retinal detachment I had come in. Frustratingly, that turned out not to be the case and instead I was sent to a surgeon: Erin Flynn, M.D. an instructor in ophthalmology at Columbia University Irving Medical Center (CUIMC).
What caused my retinal detachment
Dr. Flynn finally explained what was going on: I had what’s known as rhegmatogenous retinal detachment (RDD), the most common type of retinal detachment. Somehow, I got little holes in my cornea that caused fluid to leak in and get trapped under my retina—the light-detecting tissue at the back of my eye—and detach it.
Dr. Flynn told me that I was going to have to have surgery later that week and gave me a few things I could do before then to help limit the amount of tearing, which included lying on my right side, watching TV without closed captions and not reading or writing—which was quite difficult for me as a journalist who focuses on books and entertainment.
The day of the surgery

I don’t remember much about the day of the surgery. It was at 8 a.m., and my cousin Lauren came with me. The doctors put on songs by my favorite artist, Taylor Swift, and the next thing I knew I was awake in a different room.
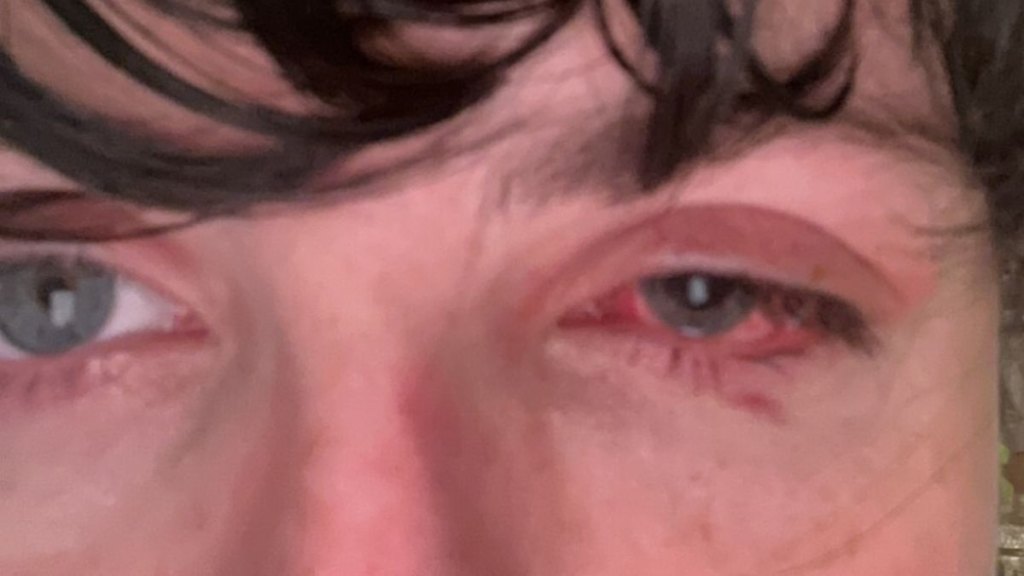
According to my cousin, the surgery took about three hours, and according to Dr. Flynn, it went perfectly. The rest of the day I was tired and had tape all over my face. I could feel the stitches in my eye but they weren’t painful, just uncomfortable. I spent most of it asleep, and when I was awake, I was on the phone answering various calls and texts, letting people know how it went.
Recovering from retinal detachment

The next week was probably one of the worst weeks of my life. I was depressed, my body was exhausted, my eye hurt, I couldn’t work and I had to lay around in the dark wearing blackout glasses. I did rewatch all eight Harry Potter movies four times, which was a silver lining but also a lot of Hogwarts. (Though you can see from my writing that I’m a fan.)
After a full week, the day before my birthday, Dr. Flynn gave me the best present: she finally cleared me to resume reading and working!
This was just the beginning of a long journey. For the next two months, I couldn’t wear a contact lens in my right eye because it was still healing, which made it hard to see. I also couldn’t wear glasses, because they were no longer the correct prescription.

Slowly but surely, my eye started to de-swell, which Dr. Flynn, said meant my eye was healing. They were still concerned with the amount of fluid that remained underneath my retina, but by the grace of God, it did drain, sparing me from another surgery.
My peripheral vision was also coming back, filling me with a sense of hope that I hadn’t felt in a long time. Perhaps the best day of my life, though, came when Dr. Flynn said I could put a contact back in my eye.
But it wasn’t quite the happy ending I wanted: When I got fitted for contacts, I realized that suddenly, there were two of everything, and they were unsure why. Dr. Flynn referred me to a double vision specialist, who’s currently helping me retrain the muscles in my right eye to snap it back in place. For now, I am just going to try and be happy that I have my vision back!

What to do if you notice retinal detachment symptoms
While retinal detachment is relatively rare, it’s important to be aware of the symptoms and seek medical treatment promptly if something seems amiss. The one thing to takeaway from my story is responding quickly to symptoms that didn’t feel right spared me my vision. Symptoms of retinal detachment include:
- A sudden increase in eye floaters
- Bright flashes of light
- Shadows in your vision
- Loss of peripheral vision
- Blurred vision.
People at an increased risk of retinal detachment include older adults, those who have had an eye injury, those with a family history of retinal detachment and those who have previously had eye surgery. Or, in my case, you can have none of these, so it’s always good to get a regular eye exam every year and talk to your doctor about your risk factors.




