The fragile structure of p53 gene reveals why this crucial cancer defense is so easily compromised, shedding light on the genetic Achilles’ heel of many tumors.
 Perspective: TP53: the unluckiest of genes? Image Credit: Juan Gaertner / Shutterstock
Perspective: TP53: the unluckiest of genes? Image Credit: Juan Gaertner / Shutterstock
In a recent perspective published in the journal Cell Death and Differentiation, researchers in France, Germany, and Sweden discussed the unique mutational spectrum of the transformation-related protein 53 (TP53) gene, which leads to p53 inactivation in many cancers.
Background
The traditional view of cancer development, driven by oncogene activation and tumor suppressor loss, has expanded to include genes involved in deoxyribonucleic acid (DNA) repair and immune escape.
Oncogenic mutations often involve single nucleotide substitutions at specific hotspots, leading to hyperactive or gain-of-function variants. Tumor suppressor mutations typically involve indels, splicing, or nonsense mutations distributed throughout the gene.
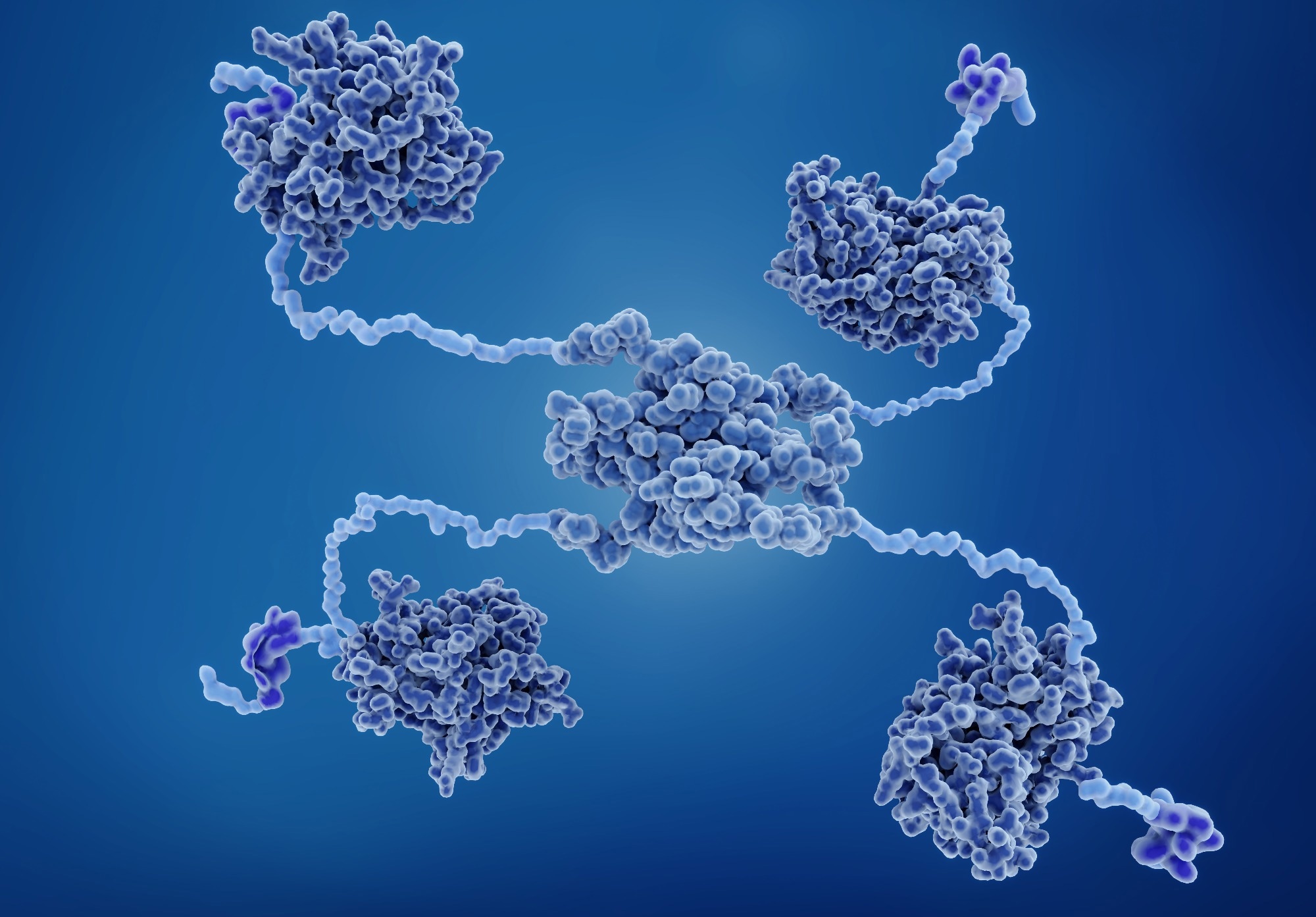
The TP53 gene is unique, with most mutations being missense and concentrated in the DNA-binding domain (DBD), possibly due to evolutionary pressures favoring a protein that balances flexibility and functional responsiveness over stability. This fragility allows p53 to adapt to cellular perturbations, but also makes it prone to mutations.
While the high expression of missense p53 variants in human tumors may have clinical significance, researchers in the present study discuss how the predominant factor shaping this mutational landscape is the extreme structural fragility of the p53 protein, influenced by its rapid evolutionary development compared to its paralogs.
p53’s Structural Fragility and its Implications
p53 mutants undergo conformational changes initially observed through chaperone binding and monoclonal antibody reactions.
Structural studies classified common TP53 mutations into two types: contact mutations, which affect DNA-binding amino acids, and structural mutations, which destabilize the protein’s DBD.
Additionally, certain mutations, like R175H, impair zinc binding, which is crucial for DBD stability. The p53 DBD is not only intrinsically unstable but also thermodynamically sensitive, making it highly sensitive to mutations and temperature shifts, which can lead to protein unfolding and loss of function. This fragility is hypothesized to be a consequence of p53’s evolutionary need to maintain a flexible conformation for rapid cellular adaptation.
Functional Analyses of TP53 Variants
Studies on TP53 saturation mutagenesis, particularly a landmark 2003 study by C. Ishioka’s group, showed that most missense mutations in TP53’s DBD cause a loss of the protein’s transactivation activity, which correlates with mutations found in human tumors.
Saturation mutagenesis revealed that over half of TP53 missense variants lead to a loss of function, similar to indel variants. Missense variants not found in cancer often retain some residual activity, and outlier mutations linked to cancer sometimes involve splice alterations.
The strong correlation between loss of function and cancer mutations highlights the role of functional impairment in cancer development, emphasizing that in most cases, these mutations lead to a reduction in tumor suppression rather than the acquisition of novel oncogenic functions.
Dominant-Negative Effect Mechanisms Worsen the Effects of Loss-of-Function Mutations
Several factors make p53 more vulnerable to inactivation compared to other tumor suppressors.
First, p53 forms tetramers, and missense mutations in its DBD have a dominant-negative effect. They form mixed tetramers that weaken DNA binding, reducing the functional wildtype p53 and compromising tumor suppression.
Additionally, unstable p53 mutants expose aggregation-prone motifs, leading to coaggregation with wild-type p53 and other proteins like p63 and p73, further hindering tumor suppression. Some gain-of-function phenotypes of mutant p53 may result from the loss of multiple functions rather than novel functions.
This aggregation effect, alongside impaired tetramer formation, underscores the complex role of mutant p53 in cancer development. Instead of introducing new cancer-driving functions, these mutants often disrupt multiple pathways, further diminishing p53’s effectiveness as a tumor suppressor.
Mutant p53 is often overabundant in tumor cells due to disrupted degradation pathways. This excess mutant protein can actively contribute to tumor progression through coaggregation and promiscuous interactions, especially in advanced cancers with genetic alterations like aneuploidy.
However, p53 loss of function, rather than its mutation status alone, remains a stronger predictor of cancer prognosis.
Selection of TP53 Mutations in Cancer
Specific mutational hotspots for TP53 missense variants in the DBD are observed in cancer. This is partly due to the high susceptibility of certain DNA sequences to mutagenic processes and environmental factors. These hotspots do not necessarily indicate a gain of oncogenic function but rather reflect the protein’s intrinsic fragility and vulnerability to the mutagenic environment.
Most TP53 missense mutations in cancer lead to a loss of function, and the prevalence of individual variants aligns with mutational likelihood and immune system recognition.
Functional studies show that removing mutant TP53 does not affect cancer growth, supporting the view that TP53 mutations primarily impair tumor suppression rather than driving new oncogenic functions.
Additionally, some hotspot mutations are less immunogenic, suggesting that immune evasion plays a role in their selection, further complicating the relationship between mutation prevalence and cancer-driving effects.
The frequency of TP53 mutations varies by tumor type and can be influenced by cell-specific factors and co-mutated oncogenes, which interact with mutant p53 to enhance cancer progression.
TP53 and its Evolutionary Past
The diversity of oncogenic TP53 variants primarily arises from the protein’s fragile and extended functional domain, making it susceptible to frequent single nucleotide substitutions (SNS) in both normal and tumor cells. While in vitro studies and mouse models suggest that some variants may exhibit diverse antimorphic or neomorphic activities, their clinical relevance remains uncertain.
The rapid evolution of p53 compared to its more stable paralogs, like p63 and p73, has contributed to its unique instability. This instability, while advantageous for its functional adaptability, makes p53 particularly susceptible to mutations.
Typically, protein structures are resilient to sequence changes, having evolved for optimal function rather than stability. The extreme fragility of p53 may enable it to adapt its conformation to cellular perturbations and allow for rapid turnover. Unlike its more stable paralogs, p53 has evolved more quickly, affecting its stability. In vertebrates, there’s a correlation between the thermodynamic stability of p53’s DNA-binding domain and the organism’s body temperature, indicating that human p53 has evolved to be only marginally stable, which contributes to its vulnerability to mutations.
Conclusion
In conclusion, the study highlights how p53’s evolutionary structure makes it particularly vulnerable to mutations that impair its tumor-suppressive function. This vulnerability is not merely a consequence of genetic instability but reflects a complex balance between adaptability, structural fragility, and evolutionary pressures.