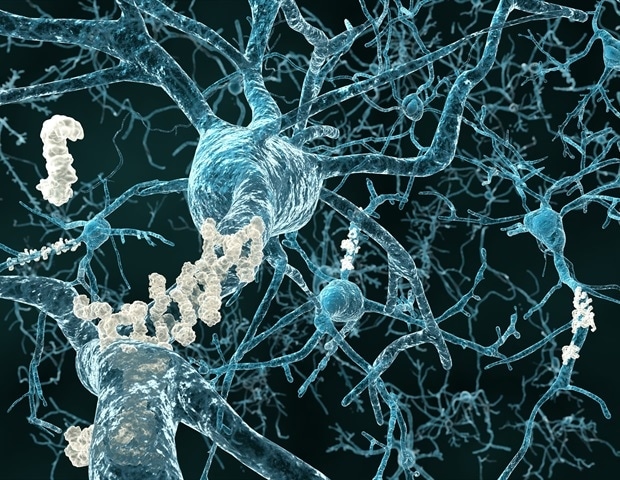
Ketone bodies, produced by the body to provide fuel during fasting, have roles in regulating cellular processes and aging mechanisms beyond energy production. Research at the Buck Institute shows that ketone bodies can best be understood as powerful signaling metabolites affecting brain function in aging and Alzheimer’s disease. A new study demonstrates that ketone bodies and similar metabolites have profound effects on the proteome and protein quality control in the brain. Publishing in Cell Chemical Biology, Buck Institute scientists, working in mouse models of Alzheimer’s disease and aging, and in the nematode C. elegans, reveal the ketone body β-hydroxybutyrate interacts directly with misfolded proteins, altering their solubility and structure so they can be cleared from the brain through the process of autophagy.
Previous studies have shown that boosting ketone bodies through diet, exercise and supplementation can be good for brain health and cognition, both in rodents and humans. Senior author John Newman, MD, PhD, an assistant professor at the Buck, says many theorized that the ketone body-based improvements were caused by increased energy to the brain or a reduction in brain inflammation, with reported improvements in amyloid plaques in mouse models being an indirect by-product.
Now we know that’s not the whole story. Ketone bodies interact with damaged and misfolded proteins directly, making them insoluble so they can be pulled from the cell and recycled.”
John Newman, Assistant Professor, Buck Institute for Research on Aging
While acknowledging that other mechanisms like energy supply are also important to brain health, Newman calls the discovery new biology. “It’s a new link between metabolism in general, ketone bodies and aging,” he said. “Directly linking changes in a cell’s metabolic state to changes in the proteome is really exciting.” Noting that ketone bodies are easy to manipulate experimentally and therapeutically, Newman adds, “This might be a powerful avenue to assist with global clearing of damaged proteins. We’re just scratching the surface as to how this might be applied to brain aging and neurodegenerative disease.”
In addition to testing the changing solubility and structure of proteins in test tubes, the project also involved feeding a ketone ester to mice to confirm that the test tube results were reproduced in the brain. In mice, the ketone ester treatment resulted in clearance rather than pathological aggregation of insoluble proteins.
The work also highlights the power of the Buck’s collaborative environment. The Schilling lab generated detailed proteome-wide solubility maps from both the test tube and mouse experiments. To test if the solubility changes caused by ketone bodies helped improve models of pathological aggregation, the Lithgow lab fed ketone bodies to tiny nematode worms that were genetically modified to express the human equivalent of amyloid beta, which causes amyloid plaques. “The amyloid beta affects muscles and paralyzes the worms,” says Sidharth Madhavan, a PhD candidate and lead author on the study. “Once they were treated with ketone bodies the animals recovered their ability to swim. It was really exciting to see such a dramatic impact in a whole animal.”
Madhavan is now pursuing whether ketone bodies and related metabolites have similar effects outside the brain, such as in the gut. A key next step will be to test this new protein quality control mechanism in people to help guide how best to apply it in therapies, he adds.
Newman says the study highlights a new form of metabolic regulation of protein quality control. “This is not just about ketone bodies,” he said. “We tested similar metabolites in test tubes and a bunch of them had similar effects. In some cases, they performed better than β-hydroxybutyrate. It’s beautiful to imagine that changing metabolism results in this symphony of molecules cooperating together to improve brain function.”
Source:
Journal reference:
Madhavan, S. S., et al. (2024) β-hydroxybutyrate is a metabolic regulator of proteostasis in the aged and Alzheimer disease brain. Cell Chemical Biology. doi.org/10.1016/j.chembiol.2024.11.001.