Your heart is a muscle. As Dr. Noah Moss, an advanced heart failure and transplant cardiologist at the Mount Sinai Fuster Hospital in New York City, puts it, “a very special muscle, but a muscle.”
Hypertrophic cardiomyopathy, or HCM, is a genetic disease in which the heart muscle grows thicker than normal. You might think of the term “big-hearted” to connote something good, says Dr. Matthew W. Martinez, director of Atlantic Health System Sports Cardiology at Morristown Medical Center in Morristown, N.J., and a nationally recognized expert in HCM. But with this condition, “there’s too much of a good thing, and that extra thickness leads to the problems associated with this disease,” he explains. The heart is inefficient (it doesn’t squeeze out enough blood), and obstruction in the heart cavity leads to murmurs that can worsen with exercise, make you breathless, and create electrical changes inside the heart.
Here’s what to know about how cardiologists diagnose the condition.
What Is Hypertrophic Cardiomyopathy?
HCM can manifest in childhood, adolescence, or any time in adulthood.
Doctors typically divide the condition into two forms: obstructive (oHCM) and non-obstructive (nHCM). The obstructive form, which represents about two-thirds of the entire HCM population, occurs when the mitral valve moves abnormally, in a manner that causes obstruction of blood flow between the heart and the aorta. “Both forms can cause shortness of breath, which worsens with exertion,” says Dr. Ronald Wharton, director of the Hypertrophic Cardiomyopathy Program, Cardiovascular Institute, Northwell Health at North Shore University Hospital in Manhasset, N.Y. “The obstructive form also causes lightheadedness that can be worsened with exertion, bending down, or a rapid change in position, [such as] quickly standing up.”
Unfortunately, HCM often flies under the radar since its symptoms aren’t unique to the disease. “Not all patients have a murmur, and not all patients who have a murmur will have one when they are sitting on an examination table,” says Wharton. “If efforts are not made to elicit the murmur—often the case in a busy office—the physical exam can easily miss the diagnosis.” (The most common way for doctors to elicit a murmur is the “Valsalva” maneuver, in which patients are asked to breathe out while they pinch their nose or asked to “bear down as if having a bowel movement.”)
HCM is important to diagnose in a timely manner to prevent the development of clinical manifestations of the disease, such as shortness of breath with walking, lightheadedness, or the feeling of intense heart beating, says Moss. Then, in rare cases—about 1% of those with HCM —the disease is associated with sudden cardiac death due to abnormal heart rhythms that result in the heart ceasing to beat effectively. (According to Martinez, the risk of sudden death from HCM can rise in some groups, such as younger people, those with a family history of sudden cardiac death, and those with scar tissue by MRI of the heart.)
Read More: What to Know About Hypertrophic Cardiomyopathy in Kids
If you’re a patient who has a very high risk of sudden cardiac death, Moss explains that your care team will recommend the implantation of a defibrillator, which is a device that continuously monitors the heart and can shock it out of a deadly arrhythmia if it detects it. Still, Martinez reassures individuals that this is a disease with normal longevity. “Most people live well into their 80s with the disease,” he says. “The majority of people live a healthy life. You can still exercise, you can still participate in life, but you do need to be seen [regularly by a cardiologist].”
HCM is typically diagnosed when evaluating the symptoms associated with the disease, or after an abnormal electrocardiogram (EKG). Typically, EKGs are administered during a routine wellness visit or for evaluation of an HCM symptom, or during screening of family members of people with HCM, says Moss. (Screening of first-degree relatives—a person’s parent, sibling, or child—is recommended after a family member is diagnosed with HCM.)
The earlier you know you have HCM, the sooner you can start treatment. Seeing a cardiologist for regular check-ups is essential, experts agree—especially if a family member has the disease or you’re exhibiting symptoms associated with HCM.
Why it Goes Undiagnosed
HCM affects roughly 1 in 250 to 1 in 500 people. Unfortunately, not everyone who has HCM is aware of it, especially because a large portion of those with HCM are asymptomatic. “About a million people in the United States carry the disease, but only 150,000 have a diagnosis. So that tells us about 85% of the time, it’s missed,” says Martinez. “It’s hiding in plain sight.”
Symptoms such as breathlessness, exercise intolerance, and feeling like your heart is racing can happen over a long period of time. That can lead to what Martinez calls “insidious disease onset.” “You say, ‘Hey, I’m just older. I’m out of shape. I don’t exercise as much.’ And you ignore it,” he says.
Wharton echoes this sentiment, noting that the available data suggest patients often go undiagnosed for three to five years following the onset of symptoms.
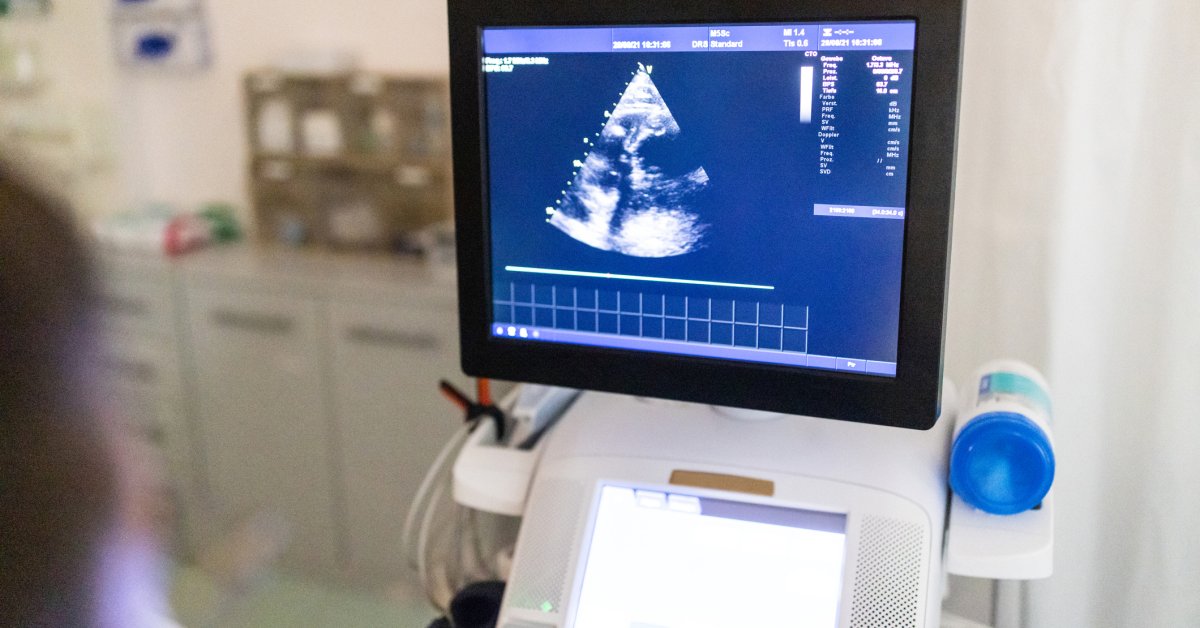
Echocardiogram
Echocardiograms, which are about 90% effective at finding HCM, are the first-line standard when it comes to diagnosing the disease. While an abnormal EKG is often the first sign of HCM, doctors make the official HCM diagnosis off an echocardiogram, often called an echo.
An echocardiogram is also the most practical way to diagnose HCM. “It is commonly available, provides information on both structure and function, is relatively inexpensive, well-tolerated, and performed without significant risk to the patient,” says Moss. After you’ve been diagnosed with HCM, echos have the additional benefit of helping doctors assess how you’re responding to treatment.
Read More: 9 Weird Symptoms Cardiologists Say You Should Never Ignore
Adds Wharton:“[An echo] is superb not just for assessing the anatomy, but also assessing the changes in the pressures within the heart chambers.”
Think of an echo as an ultrasound of your heart. “It allows us to basically see through the chest wall and visualize the heart and the flow of blood through it. We can measure the thickness of the heart muscle, see what area of the heart is affected, and see if and how the thickness is impacting the normal heart function,” explains Moss. The exam takes about 40 minutes as you lie on a table in a darkened room with heartbeat-monitoring sensors attached to your chest. Then, a cardiac sonographer applies gel to your chest and uses a probe, called a transducer, which creates moving images of your heart and other structures in the chest. It doesn’t hurt: “All you feel is the cool gel on your chest and pressure from the transducer,” says Moss.
Cardiovascular MRI
Cardiac magnetic resonance imaging, or a cardiovascular MRI, is another valuable tool in diagnosing HCM. After receiving an abnormal EKG, an echo is often the first line of evaluation for patients, but some people will still need a cardiac MRI to confirm the diagnosis, says Martinez.
In general, a cardiac MRI usually confirms the HCM diagnosis previously determined by an echocardiogram. “Its use is primarily to assist in assessing risk for dangerous heart rhythms. It can also sometimes find other diagnoses of other, often rarer conditions which can masquerade as HCM,” adds Wharton, such as cardiac amyloidosis and Danon disease.
Read More: How Hypertrophic Cardiomyopathy Progresses in Adults
“During the MRI, you lie on a bed that moves inside a tube-shaped scanner,” says Moss. “You’ll need to lie still and hold your breath for some parts of the scan.” It’s painless, but some patients can experience claustrophobia during the test, he says, noting that it can take up to 90 minutes to complete the study.
Why a Diagnosis Doesn’t Spell Doom
After comprehensive assessment, most of the time, medications for symptom relief and monitoring help patients. Asymptomatic patients can usually start with just monitoring.
If you were recently diagnosed with HCM, keep in mind that it shouldn’t prevent you from leading a healthy and active life. In fact, in 2023, Martinez and his colleagues saw about 2,000 patients with HCM, some of whom were Division 1 college athletes or professional athletes, including a number of NBA and NFL players.
“We have lots of great outcomes,” says Martinez. “My favorite thing to hear from patients when they leave the room [is], ‘I feel so much better about this disease than I did when I came here.’ And we literally have that every single day.”




