Scientists discover how the Fas-p53 pathway sabotages energy metabolism, offering new hope for tackling obesity and improving insulin sensitivity.
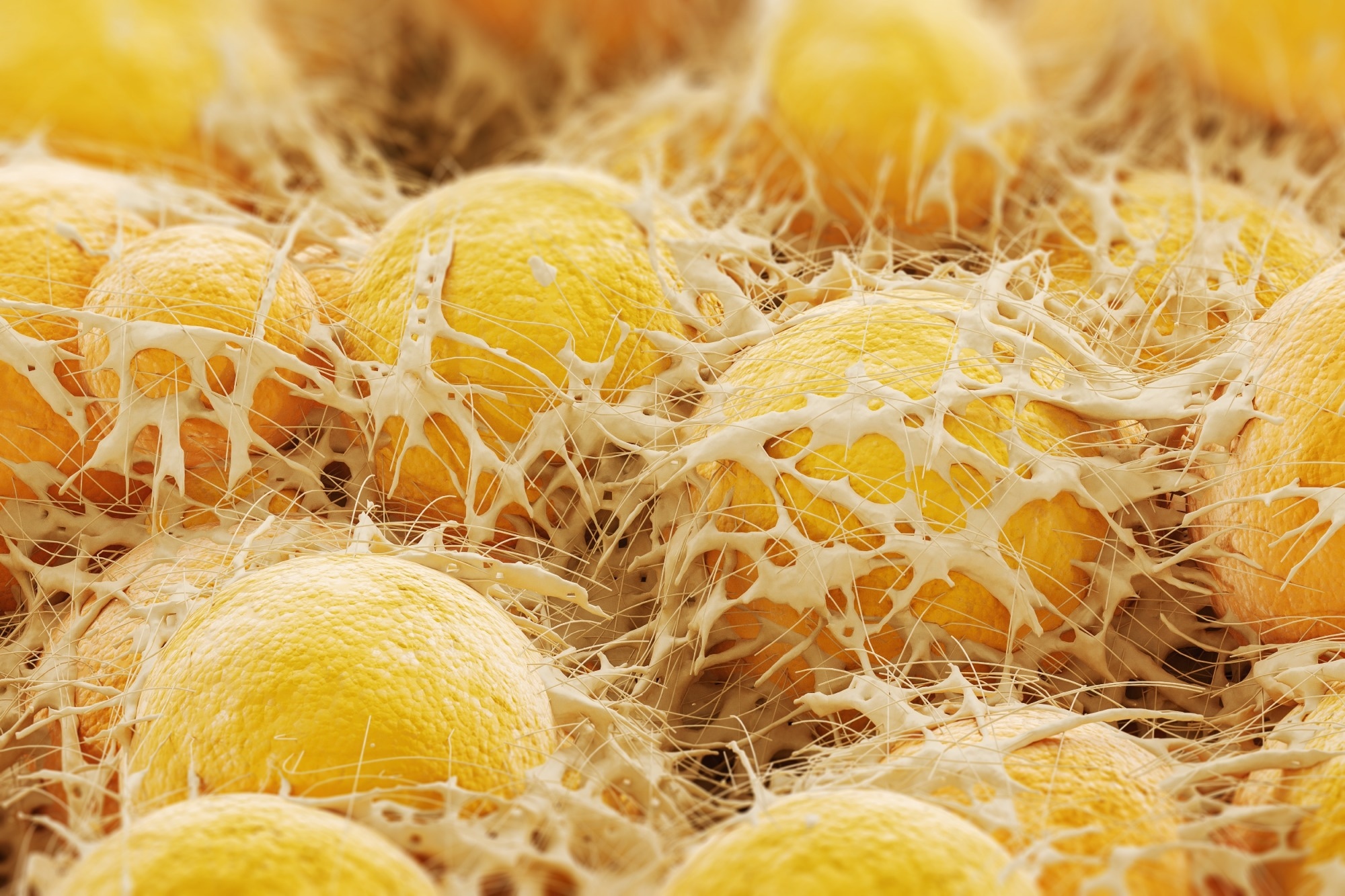
Brief Communication: Expression of p53 in human adipose tissue correlates positively with FAS and BMI. Image Credit: KateStudio / Shutterstock
In a Brief Communication published in the International Journal of Obesity, a group of researchers investigated the role of Fas Cell Surface Death Receptor (FAS) in regulating Tumor Protein p53 (p53) expression in adipocytes and its impact on energy metabolism, body weight gain, and insulin sensitivity.
Background
Adipocyte-expressed p53 (CD95) has been identified as a potential therapeutic target for reducing obesity and its associated diseases. Studies using high-fat diet (HFD)-fed adipocyte-specific Fas knockout mice have shown a dual impact: reduced inflammation and enhanced energy metabolism, including increased browning of white adipose tissue (WAT), improved insulin sensitivity, and higher whole-body energy expenditure. Similarly, FAS expression in human WAT correlates positively with adiposity, suggesting its detrimental effects are conserved across species. The tumor suppressor p53, also elevated in WAT of obese mice and humans, may contribute to inflammation, insulin resistance, and reduced energy expenditure. Further research is needed to explain Fas and p53 interplay in metabolic regulation.
About the study
Paired abdominal and femoral subcutaneous adipose tissue (AT) biopsies from 18 postmenopausal women (Body mass index (BMI): 21.2-40.6 kg/m², age: 50-62 years) were analyzed for p53 messenger RNA (mRNA) expression. Ethical approval was granted by the United Kingdom (UK) Health Research Authority, and participants provided written informed consent.
In a cross-sectional study of 302 individuals (205 women, 97 men; BMI: 16.9-85.5 kg/m², age: 16-90 years), FAS and p53 mRNA expression were assessed in subcutaneous and visceral WAT collected during elective laparoscopic surgery. Hyperinsulinemic-euglycemic clamps were conducted in a subset of participants. Ethical approval was obtained from the University of Leipzig Ethics Committee, and all procedures adhered to the Declaration of Helsinki.
White adipocytes isolated from 26-week-old HFD-fed Fas knockout mice underwent mitochondrial oxygen consumption rate (OCR) analysis. Differentiated adipocytes treated with Fas ligand (FasL) or vehicle were subjected to sequential treatments using isoproterenol, oligomycin, and antimycin A, measured via Seahorse XF Pro Extracellular Flux Analyzer. Data were analyzed using Regression and Outlier Removal (ROUT) and calculated using the manufacturer’s equations.
GraphPad Prism software was used for statistical analyses. Shapiro-Wilk, Mann-Whitney, and Student’s t-tests were applied for group comparisons, while Analysis of Variance (ANOVA) and Spearman correlation analyzed multi-group differences and linear relationships, respectively.
Study results
The role of Fas in regulating p53 levels in adipocytes was investigated using adipocyte-specific Fas knockout mice. Primary adipocytes isolated from these mice displayed significantly reduced p53 protein abundance compared to controls when fed an HFD, as shown through Western blot analysis. Conversely, subcutaneous white adipocytes treated with non-apoptotic concentrations of FasL exhibited a notable increase in p53 protein levels. These findings suggest that Fas positively regulates p53 protein levels in adipocytes.
To explore whether the Fas-p53 axis influences energy expenditure, experiments were conducted using Seahorse XF Pro Extracellular Flux Analyzer on FasL-treated adipocytes with or without Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9-mediated p53 knockout. Consistent with previous studies, p53 knockout significantly elevated mitochondrial OCR and was associated with reduced coupling efficiency and increased expression of uncoupling protein 1 (UCP1). Interestingly, FasL treatment significantly reduced both basal and proton leak-linked OCR in control cells but not in p53-knockout cells, reinforcing the hypothesis that Fas activation decreases energy expenditure in a p53-dependent manner.
To extend these findings to human adipocytes, FAS and p53 gene expression was assessed in differentiated human multipotent femoral and abdominal adipose-derived stem cells (hMADS). A significant positive correlation between FAS and p53 mRNA expression was observed in hMADS from both fat depots, supporting the hypothesis that Fas acts as a positive regulator of p53 in human adipocytes.
Further investigation examined the relationship between p53 expression in human WAT and measures of obesity and insulin resistance. A positive correlation between FAS and p53 mRNA expression was confirmed in both abdominal subcutaneous and visceral WAT. Moreover, p53 and FAS expression levels in these depots were shown to correlate positively with BMI and negatively with glucose infusion rates (GIR), a key marker of insulin sensitivity, during hyperinsulinemic-euglycemic clamps. Additionally, p53 expression in both WAT depots was negatively associated with UCP1 expression, suggesting that p53 may attenuate thermogenic capacity.
Conclusions
The findings suggest that Fas regulates p53 levels in adipocytes, negatively impacting body weight gain and glucose metabolism. Fas activation increases p53 levels, while Fas depletion reduces them, with positive correlations between FAS and p53 observed in human WAT and adipose-derived mesenchymal stem cells. Elevated Fas expression in obese mice and humans parallels increased p53 levels, which correlates positively with BMI. Seahorse analysis revealed that p53 depletion enhances mitochondrial oxygen consumption, while Fas activation reduces it in a p53-dependent manner, potentially linked to lower UCP1 levels. These results indicate that the Fas-p53 pathway could serve as a potential therapeutic target for addressing obesity-related metabolic dysfunction.