During perimenopause, a decline in your body’s estrogen levels can lead to symptoms like hot flashes, mood swings, vaginal dryness, decreased libido and more. While hormone replacement therapy (HRT) in the form of tablets, patches and implants can help alleviate that broader discomfort, localized vaginal estrogen specifically targets “down there” bothers. Here, a doctor shares the benefits of vaginal estrogen, how to talk to your physician about it and why it’s a safe treatment option for many women.
What is vaginal estrogen?
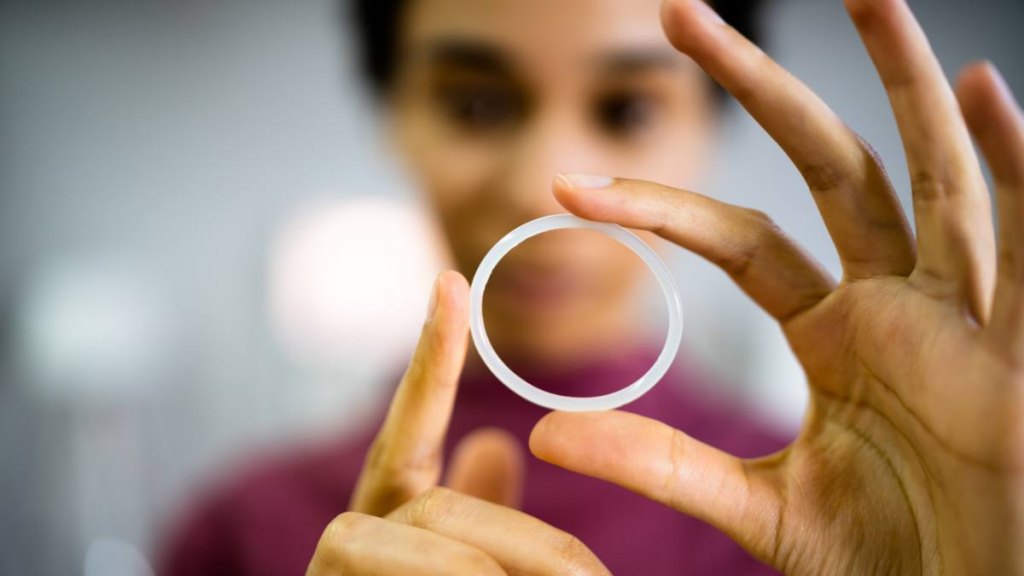
Vaginal estrogen is like a local delivery system for something your body naturally needs, explains Christine Maren, DO, founder of a functional medicine practice focused on women’s health and hormones. “It’s a targeted hormone therapy that works specifically in the genitourinary system, unlike systemic hormone therapy, which affects your whole body,” she explains. You can find it in various forms, including creams, inserts or rings. It provides a small dose of estrogen therapy directly where you need it.
Would you ever consider using vaginal estrogen?
When should you consider vaginal estrogen?
Perimenopause and menopause bring out many emotional, physical and mental changes, which is why Dr. Maren believes vaginal estrogen is your secret weapon during this time. “It helps maintain vaginal health, tissue elasticity and natural lubrication when your body’s estrogen production starts declining,” she says. Since these fluctuations can start as early as your late 30s or early 40s, finding a treatment that works for you sooner rather than later can help you avoid some of the most bothersome perimenopause symptoms.
“Vaginal estrogen is most helpful (and can actually save lives!) during menopause when estrogen levels really wane, but can also help perimenopausal women, especially when they are struggling with urinary incontinence, painful intercourse, recurrent UTIs or vaginal yeast infections,” adds Dr. Maren.
The benefits of vaginal estrogen
Dr. Maren is quick to point out that using vaginal estrogen isn’t just for those going through perimenopause or menopause. Anyone with low estrogen levels can try it to improve their overall vaginal and urinary health. Here, the health benefits of vaginal estrogen:
It improves vaginal dryness and discomfort
Vaginal dryness is a relatively common symptom of genitourinary syndrome of menopause (GSM). By using vaginal estrogen, you can restore collagen, elastin and hyaluronic acid in the vaginal tissues, which improves hydration, says Dr. Maren. She adds that this results in increased natural lubrication and comfort, especially for women experiencing vaginal atrophy due to estrogen deficiency.
It balances your vaginal pH
A normal vaginal pH falls between 3.5 and 4.5—leaning towards the acidic side of the spectrum—and this is the best level for healthy bacteria. “Estrogen promotes the proliferation of lactobacillus, the ‘good’ bacteria that help maintain a healthy vaginal ecosystem,” says Dr. Maren. “Lactobacilli produce lactic acid, which lowers vaginal pH to acidic levels (typically below 4.5).” This can help reduce your risk of itchy, vaginal discharge and other bothersome symptoms that occur when your vaginal pH is disrupted.
It boosts your libido

While a reduced sex drive is common during perimenopause or menopause, it doesn’t have to be the norm. In fact, Dr. Maren says estrogen thickens the outer tissue and improves blood flow and elasticity, which restores the natural resilience of vaginal tissues, making sexual activity far less painful. The result? When intercourse isn’t uncomfortable anymore, your libido may start to rise again.
Not only does estrogen aid with pain during intercourse, it also helps with arousal. “By improving blood flow to the vaginal and vulvar tissues, estrogen increases sensation and enhances natural lubrication,” says Dr. Maren. “Together, these factors reduce discomfort and promote greater sensitivity and arousal during intimacy.”
It reduces the risk of UTIs
Research shows that vaginal estrogen significantly reduces recurrent urinary tract infections (UTIs) by more than 50 percent. Why? “Estrogen supports a healthy vaginal microbiome (which inhibits pathogenic bacteria like E. coli) and reduces vaginal atrophy, which can lead to microscopic tears and urethral irritation during sex”—all of which raise the risk of UTIs, says Dr. Maren
It reduces bladder leaks
“Vaginal estrogen helps with urgency, frequency and mild incontinence by strengthening [pelvic muscles] and improving the elasticity and thickness of the bladder neck and vaginal walls,” explains Dr. Maren. She adds that this is especially beneficial to those who’ve experienced pelvic floor changes due to childbirth or menopause.
How to talk to your doctor about the benefits of vaginal estrogen
Dr. Maren says the best thing to do if you are interested in trying vaginal estrogen is to be direct with your doctor or other healthcare professional. “Start with something like, ‘I’ve been experiencing vaginal dryness/urinary issues/discomfort during intimacy, and I’ve heard vaginal estrogen might help. I’d like to consider this treatment option,’” she says. She also notes that it’s important to ask the right questions. These include:
- Which form (cream, insert or ring) would work best for my lifestyle?
- How often should I use it?
- How long before I might notice improvements?
- Are there any specific applications or techniques I should know about?
- Should I use it in combination with my current medications/treatments?
- What symptoms should I track to know if it’s working?
Vaginal estrogen is safe to use
According to the new Let’s Talk Menopause campaign, vaginal estrogen has been deemed safe and effective in multiple studies. Because of this, proponents urge the U.S. Food and Drug Administration (FDA) to remove the boxed warning—a warning that appears on the label of certain prescription drugs to alert consumers and healthcare providers to serious risks—label from local vaginal estrogen.
“Unlike systemic hormone therapy, it works locally and has no increased risk of blood clots, stroke or heart disease,” adds Dr. Maren. “Even better? It’s generally considered safe for women with a history of breast cancer (though always consult your healthcare provider for personalized advice).”
This content is not a substitute for professional medical advice or diagnosis. Always consult your physician before pursuing any treatment plan.




