In this interview, discover how retina models are revolutionizing rare disease treatment and accelerating drug development.
What are the biggest challenges in developing effective therapies for rare and ultra-rare retinal diseases?
Dr. Lauren Black: The challenges are vast. While each rare disease affects a small number of people individually, collectively, it impacts hundreds of millions worldwide. Rare diseases often have a genetic basis, with about 80 % linked to specific genetic mutations, yet 95 % lack disease-modifying treatments.
The regulatory framework and diagnostic delays add more complexity, and for ultra-rare conditions, it is hard even to find relevant literature or research. Developing therapies for such diseases requires an approach tailored to each mutation, often necessitating N=1 trials where treatments are designed specifically for individual patients.
Time is a critical factor here, as many rare diseases progress rapidly, especially in children, placing immense urgency on developing innovative models and therapies.
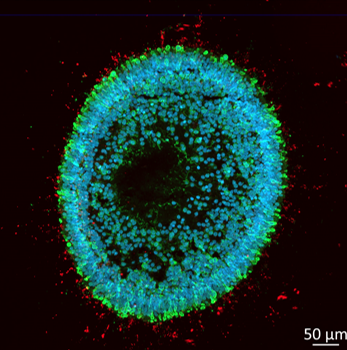
Image Credit: Newcells
How are predictive models, particularly retinal organoids, contributing to advancements in retinal disease research?
Dr. Roxana Redis: Retinal organoids have shown remarkable promise, especially in cases where traditional models fall short. These organoids are derived from patient cells and can mimic the structure and function of human retina tissue, making them excellent models for retinal diseases.
For instance, in developing treatments for specific genetic retinal diseases like Leber congenital amaurosis, retinal organoids allowed us to study the precise mutation effects in vitro.
This model was crucial, as the typical animal models did not exhibit the disease phenotype due to species-specific genetic differences. With organoids, we demonstrated proof of concept, which was then presented to regulatory authorities to help move the therapy forward to clinical trials.
Can you provide specific examples of cases where retinal organoids have provided proof-of-concept data for rare disease therapies?
Dr. Roxana Redis: One example is an antisense oligonucleotide (ASO) therapy developed for a form of Leber congenital amaurosis. The condition results from a mutation in the CEP290 gene, which leads to the inclusion of a cryptic exon and disrupts protein production, causing blindness from birth.
Although a transgenic mouse model was created, it could not replicate the human splicing defect. Patient-derived retinal organoids, however, allowed us to test the ASO therapy, restoring photoreceptor functionality in vitro. This success in retinal organoids provided essential proof of concept for regulatory approval, helping move the treatment to clinical trials.
What are the main limitations of retinal organoids, and how can researchers address issues of variability and reproducibility in these models?
Dr. Valeria Chichagova: Retinal organoids are complex and present several challenges. Their cellular makeup and structure must be controlled rigorously, especially because variability can arise from batch-to-batch differences.
To minimize this, we implement standardized protocols and strict quality control at every step—from the starting induced pluripotent stem cells (iPSCs) to the organoid differentiation process. Maintaining reproducibility also requires careful staging; different developmental stages are suited to studying different retinal diseases or therapeutic responses.
Our lab conducts thorough assessments to ensure cell composition and organization remain consistent across batches. This approach is vital for establishing retinal organoids as a reliable model in preclinical studies.
Given the complex nature of retinal organoids, how important is it to select the correct developmental stage when using these models in research?
Dr. Valeria Chichagova: It is absolutely essential. Retinal organoids go through stages paralleling human retinal development, each with unique cell types and structures.
Early-stage organoids are enriched in retinal ganglion cells, which may be ideal for studying diseases impacting those cells. Later stages develop photoreceptor cells. By day 180, photoreceptors mature with outer segments, a key structural component for vision.
Using organoids at this later stage is crucial for therapies targeting photoreceptors. Researchers must align the organoid’s developmental stage with the specific research question to ensure meaningful data and predictive validity.
How do you foresee the role of retinal organoids evolving in the regulatory landscape, especially concerning IND applications?
Dr. Lauren Black: Retinal organoids have the potential to play a greater role, but it is a gradual process. Regulatory guidelines, like those from the FDA, still favor animal models because of their historical precedence and assurance for certain biological aspects, like systemic bio-distribution.
As we build evidence on organoids’ accuracy in mimicking human disease, especially in cases where no animal models are feasible, regulators are increasingly open to considering them as part of the IND package. This is particularly true for rare diseases with limited time and patient numbers.
Ultimately, it will take ongoing collaboration between researchers, industry, and regulatory bodies to fully integrate these models into the regulatory framework.
Could predictive models like retinal organoids replace animal models entirely in preclinical studies, and what factors may support or hinder this shift?
Dr. Roxana Redis: It is unlikely that animal models will be completely replaced anytime soon. Organoids are invaluable for studying disease mechanisms and drug effects at the cellular level, but they do not capture all the complexities of an entire organism.
Understanding a drug’s bio-distribution or toxicity across multiple organ systems still requires animal testing. Retinal organoids can, however, reduce animal use by providing preliminary efficacy and safety data, especially for rare diseases with limited patient populations.
The shift will be gradual, with organoids supplementing animal studies rather than replacing them entirely.
What advice would you give to researchers looking to expedite IND submissions using alternative models such as retinal organoids?
Dr. Valeria Chichagova: My advice is to ensure your model is as robust as possible. Organoids are promising, but regulators expect consistency and reliability. Develop and validate protocols meticulously and be prepared to demonstrate the model’s translational relevance for your specific disease.
Collaborate with regulatory experts early to understand what data is essential. Finally, plan your studies strategically. Retinal organoids are not perfect substitutes for all research questions, but if used correctly, they can expedite certain aspects, like proof of concept for genetic therapies.
What progress has been made in the development of assays for photoreceptor functionality in retinal organoids, and what are the current challenges?
Dr. Valeria Chichagova: Progress is ongoing, but it is challenging. Photoreceptor functionality in organoids is difficult to measure consistently because the structure and response of photoreceptors in vitro do not fully replicate those in human tissue.
We need more sophisticated assays to accurately assess key functional units like photoreceptor outer segments. Right now, variability in functional measurements remains high across different labs, making it difficult to standardize findings. This is a critical area where we hope to see innovation soon.
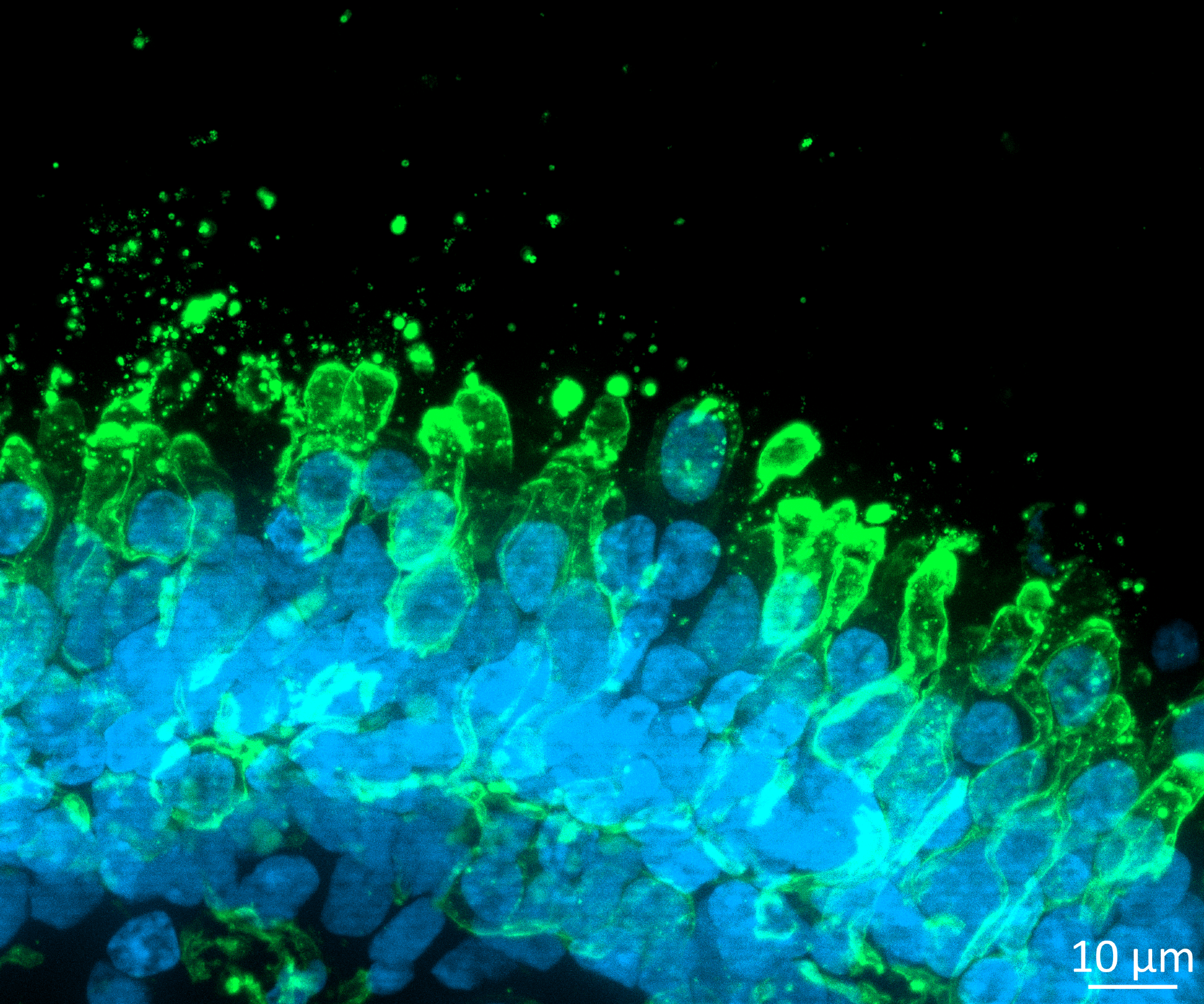
Image Credit: Newcells
How do you address the challenges of heterogeneity within retinal organoids, particularly in multi-batch studies?
Dr. Valeria Chichagova: Heterogeneity is a challenge, but we address it through rigorous quality control. It starts with carefully selecting the iPSC line and standardizing the differentiation protocol. We then monitor each stage’s cell composition and development timeline to ensure uniformity.
By continuously measuring cell type proportions and functionality, we minimize batch-to-batch variability. This is essential for reliable data and building the case for organoids as a reproducible model that can meet regulatory requirements.
How can collaborative efforts between industry and regulators advance the acceptance of in vitro models for clinical research, particularly for rare diseases?
Dr. Lauren Black: Collaboration is critical. We have seen progress in skin and eye irritation models, which are now widely accepted as in vitro tests. Similar progress with organoids will require industry groups and regulators to establish standardized protocols, conduct validation studies, and openly share data.
When multiple stakeholders agree on best practices, it accelerates acceptance. Rare diseases, where traditional models often do not apply, offer a unique opportunity for innovation. Working together, we can fast-track these models’ acceptance for rare disease research and potentially expand their use to broader areas.
What are the future possibilities for retinal organoids beyond rare diseases, and how might they be applied to more common retinal conditions?
Dr. Roxana Redis: The potential applications are significant. While rare and ultra-rare diseases are an initial focus, the insights and methodologies developed with retinal organoids could eventually be applied to more common conditions like age-related macular degeneration or diabetic retinopathy.
These organoids offer a model that mirrors human retinal biology more closely than animals, so they could be instrumental in testing therapies for a broader range of conditions. We are still in the early stages, but as the technology matures, we anticipate broader applications that could impact millions of people affected by retinal diseases worldwide.
About Newcells Biotech
Newcells Biotech develops in vitro cell-based assays for drug and chemical discovery and development.
Using our expertise in induced pluripotent stem cells (iPSCs), cellular physiology, and organoid technology, we build models that incorporate the “best biology” for predicting in vivo behavior of new drugs.
Our experts have developed and launched assays to measure transporter function, safety, and efficacy in a range of cell and tissue types, including kidney, retina and lungs.
We have the capability to develop and implement protocols to measure cilia beat frequency and toxicity on small airway epithelial cells model, retinal toxicity and disease modelling on retinal organoids and retina epithelium, as well as drug transport in the kidney, DDI and nephrotoxicity across human and a range of preclinical species.




