Arteriovenous malformations, a hallmark of hereditary hemorrhagic telangiectasia, may be driven by endothelial cell-cycle acceleration via CDK6, suggesting potential for repurposing CDK6 inhibitors.
A recent study published in Nature Cardiovascular Research suggests that inhibiting endothelial cell (EC) proliferation is a potential treatment for hereditary hemorrhagic telangiectasia (HHT).
Background
HHT is a rare genetic disorder characterized by the loss of capillaries and abnormal artery-vein connections, viz., arteriovenous malformations (AVMs). AVMs occur in specific tissues, such as the lungs, liver, mucosa, skin, and the central nervous system. In the mucosa, these lesions are susceptible to rupture, leading to uncontrolled bleeding and chronic anemia.
HHT occurs due to heterozygous loss-of-function germline mutations in genes involved in the bone morphogenetic protein 9 (BMP9) and BMP10 signaling pathway, including endoglin (ENG), activin A receptor-like type 1 (ACVRL1), and SMAD family member 4 (SMAD4). HHT pathogenesis originates in ECs, which predominantly express ENG and activin receptor-like kinase 1 (ALK1) (encoded by ACVRL1).
In vitro studies over two decades ago demonstrated that ALK1 signaling regulates the cell cycle. The initial in vivo evidence for this emerged from BMP10 neutralization in Bmp9-deficient mice and genetic ablation of Alk1 in ECs in a mouse model. However, the mechanistic links between cell cycle dysregulation in ECs and the development of AVMs are lacking.
The study and findings
The present study demonstrated that cyclin-dependent kinase 6 (CDK6) is involved in AVM development in preclinical HHT models. The researchers used the neonatal retinal angiogenesis AVM model. They perturbed the BMP9/10 signaling pathway by EC-specific ablation of Eng (Engi–ECKO mice) or postnatal treatment with antibodies to BMP10 and BMP9 (BMP9/10ib mice).
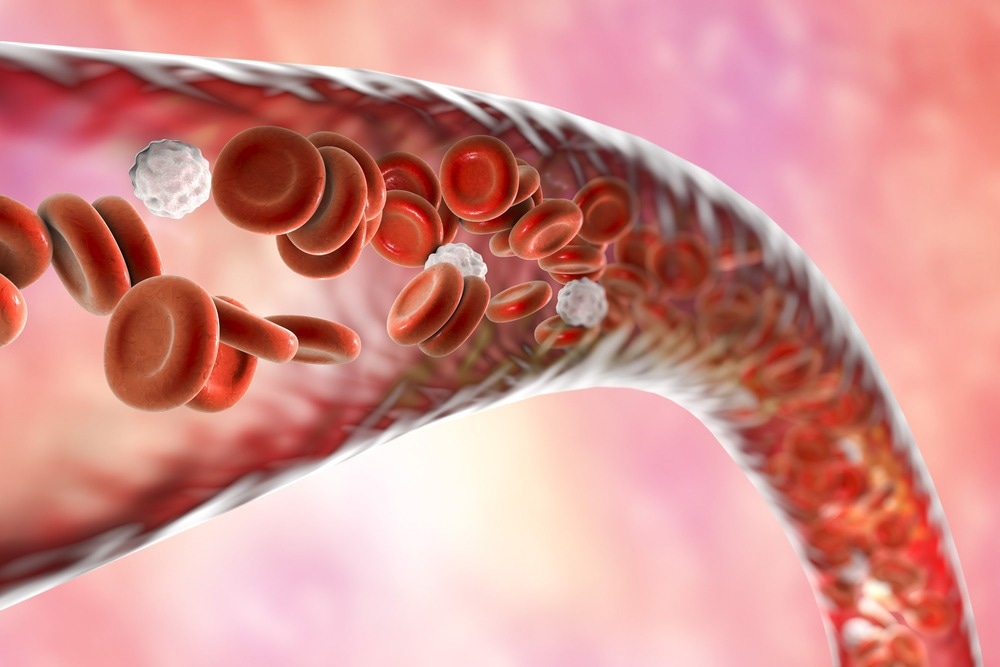
They observed active EC proliferation in retinal AVMs and liver vasculature in BMP9/10ib mice. Further, BMP9/10 inhibition caused G1/S checkpoint bypass and accelerated the cell cycle in ECs. Besides, CDK4 and CDK6 expression increased in Engi–ECKO and BMP9/10ib mice, promoting retinoblastoma protein phosphorylation (p-RB1).
Next, mice lacking endothelial Cdk6 expression were generated. This revealed that the animals were protected from retinal AVMs, hypervascularization, and vein dilation. Furthermore, the researchers tested drugs targeting CDK6 and CDK4. One drug, palbociclib, decreased established retinal AVMs, and hypervascularization was observed in the brain and liver.
The drug was also effective in preventing retinal AVM development and vasodilation in the brain and duodenum. A different study confirmed the prevention of EC proliferation and retinal AVMs by palbociclib in Smad4i–ECKO mice. Further, the researchers showed that vascular endothelial growth factor (VEGF) induces the expression of CDK6, which was inhibited by BMP9 addition.
Moreover, VEGF pathway overactivation has been suggested in HHT patients, and treatment with bevacizumab (a monoclonal antibody against VEGF) has been found to alleviate epistaxis significantly. Two hypotheses have been proposed for how an increased EC proliferation leads to AVMs. First, defects in EC cell cycle control may impact normal migration against the blood flow. Alternatively, EC cell cycle defects may impact arteriovenous specification.
In addition, the researchers observed p-RB1 immunoreactivity (as a cell proliferation readout) in the EC skin telangiectases of two HHT patients, supporting the notion of elevated EC proliferation in HHT. However, proliferative ECs represent a small pool, and whether or not they regulate AVMs in patients warrants investigation.
Conclusions
Taken together, the findings reveal the dysregulation of the cell cycle in ECs in HHT and support the idea that drugs that arrest the cell cycle could be relevant to regress/prevent vascular malformations in HHT. Currently, abemaciclib, palbociclib, and ribociclib are the approved CKD4/6 inhibitors. While these are well tolerated, they have side effects, including anemia.
Therefore, it is difficult to imagine the long-term impact of CDK4/6 inhibition on the hematopoietic system, given the predisposition of HHT patients to anemia and hemorrhaging. The study’s limitations include using preclinical neonatal HHT models characterized by active angiogenesis. Moreover, findings were limited to AVMs in the retina that do not form in humans.
Translating animal data to humans may be difficult since AVMs develop in various organs and may be affected by other mechanisms. In addition, HHT patients suffer from bleeding, which the study did not investigate in these models. Overall, additional studies are necessary to examine the clinical relevance of these inhibitors before consideration in humans.
Journal reference:
- Dinakaran S, Qutaina S, Zhao H, et al. CDK6-mediated endothelial cell cycle acceleration drives arteriovenous malformations in hereditary hemorrhagic telangiectasia. Nature Cardiovascular Research, 2024. doi: 10.1038/s44161-024-00550-9 https://www.nature.com/articles/s44161-024-00550-9